"There is a growing realization that the ways genes are regulated to work together can be important for understanding disease," said Mike Pazin, Ph.D., a program director in the Functional Analysis Program in NHGRI's Division of Genome Sciences. "The GGR program aims to develop new ways for understanding how the genes and switches in the genome fit together as networks. Such knowledge is important for defining the role of genomic differences in human health and disease."
With these new grants, researchers will study gene networks and pathways in different systems in the body, such as skin, immune cells and lung. The resulting insights into the mechanisms controlling gene expression may ultimately lead to new avenues for developing treatments for diseases affected by faulty gene regulation, such as cancer, diabetes and Parkinson's disease.

Over the past decade, numerous studies have suggested that genomic regions outside of protein-coding regions harbor variants that play a role in disease. Such regions likely contain gene-control elements that are altered by these variants, which increase the risk for a disease.
"Knowing the interconnections of these regulatory elements is critical for understanding the genomic basis of disease," Dr. Pazin said. "We do not have a good way to predict whether particular regulatory elements are turning genes off or activating them, or whether these elements make genes responsive to a condition, such as infection. We expect these new projects will develop better methods to answer these types of questions using genomic data."
Recipients of the new GGR three-year grants (pending available funds) are:
- Memorial Sloan Kettering Cancer Center, New York City, $3.2 million
Principal Investigators: Christina Leslie, Ph.D. and Alexander Rudensky, Ph.D.
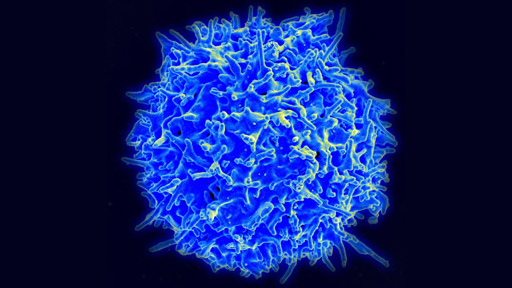
The body's immune system can cause inflammation, which plays a central role in some diseases. The investigators will use a mouse model to study genomic mechanisms underlying immune system activity during inflammation. They will determine what and when genes are turned on and off, and how they are controlled, in the development and activation of two different types of immune cells with opposite functions. One cell type promotes the immune system's response and inflammation; the other dampens these functions.
- Duke University, Durham, North Carolina, $5.9 million
Principal Investigator: Timothy Reddy, Ph.D.
Researchers will characterize how human lung epithelial cells respond to anti-inflammatory drugs called glucocorticoids (a type of steroid hormone). They will determine what and when genes are turned on and off, and how this process is controlled. They hope to create a model for this type of response, and detail the gene regulation patterns involved. This may allow the researchers to understand how glucocorticoids control both anti-inflammatory and metabolic responses.
- University of Massachusetts Medical School, Worcester, $6.1 million
Principal Investigators: Jeremy Luban, M.D. and Manuel Garber, Ph.D.
Investigators will study a type of immune cell called a dendritic cell as a model with which to explore gene regulation. This cell is part of the innate immune system that, together with the acquired immune system, distinguishes self from non-self and enables the body to react to pathogenic invaders. The researchers will examine the changes that the dendritic cell undergoes when it encounters a pathogen, including the genes that are turned on and off, molecules that are made and receptors that are activated.
- Stanford University, Stanford, California, $7.1 million
Principal Investigator: Michael Snyder, Ph.D.
Dr. Snyder and his team will study the development of one type of skin cell (keratinocyte) as it develops from an early stage skin cell into a mature cell. To do this, they will examine the network of genes and pathways that control this developmental change. The results may ultimately have implications for better understanding skin biology and hundreds of skin disorders.
- University of California, Los Angeles, $6 million
Principal Investigators: Alexander Hoffmann, Ph.D. and Douglas Black, Ph.D.
Researchers will study the immune system's response to pathogens. They will examine how a type of white blood cell called a macrophage reacts to a bacterial pathogen, which can result in the activation of more than 1,000 genes. This model system will allow the scientists to examine various steps in the gene expression pathway to try to better understand some of the control mechanisms involved.
The grant numbers of the awards are: 1U01HG007893-01; 1U01HG007900-01; 1U01HG007910-01; 1U01HG007919-01; and 1U01HG007912-01.
NHGRI is one of the 27 institutes and centers at the National Institutes of Health. The NHGRI Extramural Research Program supports grants for research and training and career development at sites nationwide. Additional information about NHGRI can be found at http://www.genome.gov.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 institutes and centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.nih.gov.